Choice of drug therapy for chronic insomnia
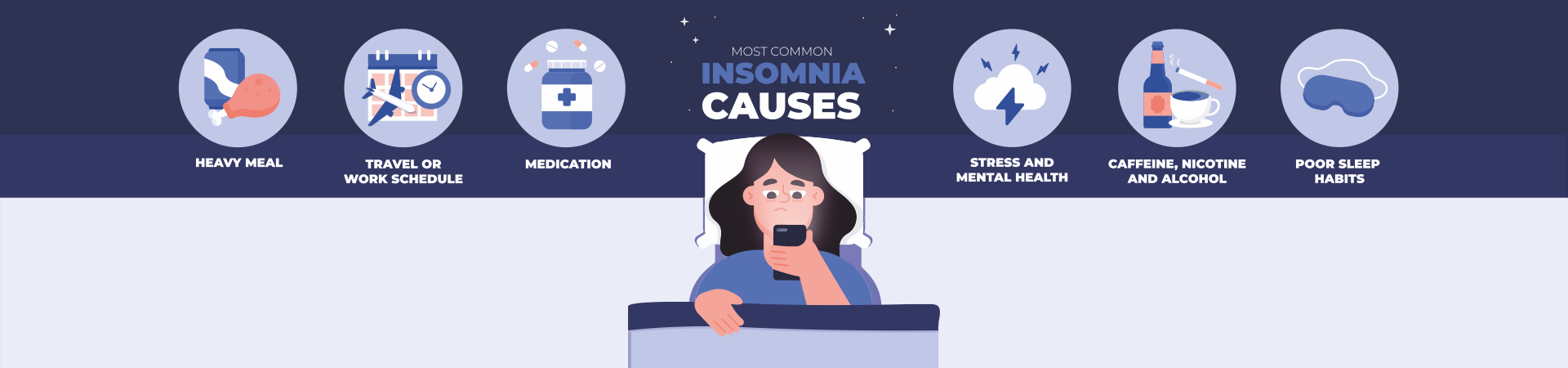
Insomnia is the most commonly spoken term by patients and healthcare professionals. However, there is still no generally accepted definition of this phenomenon. Depending on the context, the term can mean a symptom, syndrome, independent disease, or a secondary disorder caused by another physical or mental disorder. Insomnia is a condition with unsatisfactory duration and / or unsatisfactory quality of sleep for a significant period of time.
According to the duration of insomnia, it is customary to divide into three subgroups.
Transient insomnia lasts up to one week and is an adaptation disorder caused by an acute situational factor (new job, exam). Short-term insomnia lasts from several weeks to 4 months and is usually associated with a long -term traumatic situation (intractable conflict, illness) or with exogenous factors (noise). Any insomnia that lasts more than 6 months is considered chronic and is formed due to physical or mental illness.
It is now generally accepted that chronic insomnia in 80-90% of cases is to some extent associated with affective disorders – depression or anxiety disorders (1).
In 1999 , a study by scientists from the University of Washington was published in the journal Clinical Drug Investigation. It showed that 3 million US residents each year go to primary care with complaints of insufficient sleep, with a third of patients this being the only reason for the visit. Only 15% of these patients were prepared by doctors to diagnose insomnia as an independent disorder and to prescribe sleeping pills. 62% of these patients were diagnosed with a mental disorder and prescribed appropriate therapy for the underlying disease. The authors believe that about a third of the population suffers from sleep disorders, but only 5% of them seek medical help.
The severity of insomnia is determined not so much by the duration of sleep as by the influence on the quality of the patient’s functioning during the daytime wakefulness. At the same time, there are objective signs of exhaustion and asthenic complaints during the daytime, impaired concentration of attention and memory, decreased social functioning and industrial productivity.
Chronic insomnia can be:
- a risk factor for the development of a mental disorder, primarily depression;
- prodromal symptom of depression;
- a consequence or complication of depression, which lasts even after the end of a clinically delineated episode, which, in turn, is a prognostic indicator of a protracted course of affective disorder and insufficient therapeutic response.
In 95% of patients with affective disorders, insomnia is one of the 3-5 main complaints. With insomnia associated with such disorders, the most characteristic complaints of patients are:
- difficulty falling asleep;
- frequent awakening in the middle of the night;
- early morning awakening;
- a painful feeling of lack of sleep saturation;
- persistent complaints for at least a month of fatigue during the day, disruption of daily functioning (2).
Experienced clinicians note the predominance of complaints of difficulty falling asleep in patients with leading symptoms of anxiety, and early awakening in patients with dominant depressive symptoms. In recent decades, more than half of patients with affective disorders have noted both of these signs. The notion that depression leads to the formation of chronic insomnia is quite obvious. Currently, there is evidence of an inverse relationship – the presence of insomnia leads to the formation of depression. Thus, it was found that the presence of insomnia for more than a month at the age of 21-30 increases the risk of depression in the next 3-4 years by 4 times (3).
Regardless of the nosological affiliation of the emotional disorder, we can say that the degree of subjective significance for the patient of insomnia and the severity of its objective indicators are directly proportional to the severity of anxiety symptoms in the structure of affective disorder, primarily depression. In turn, the prognostic value of anxiety in the clinic of depressive conditions is associated with the following factors:
- severe initial condition;
- pronounced social and psychological maladjustment;
- a high probability of the formation of a protracted current;
- insufficient, delayed and delayed therapeutic response;
- greater risk of suicide.
Thus, the presence of chronic insomnia in a patient indicates a probable affective pathology, and the dynamics of insomnia may be one of the most important indicators of the effectiveness of therapy for emotional disorders.
Before moving on to the existing choice of therapy for insomnia as a target symptom in the structure of affective disorder, it is necessary to note some neurophysiological indicators of sleep in health and disease, as well as the effect of certain drugs on them.
The most important and most practical indicator of sleep is its performance, which is determined by the ratio of the time spent in bed to the duration of sleep. Sleep has a certain cyclical nature and normally there is a gradual, sequential transition from light nap (stage 1) to deep sleep (stage 4) within the so-called phase without rapid eye movement (non-REM phase). The cycle ends with a fairly delineated episode of the phase of rapid eye movement under closed eyelids (REM phase). Electroencephalographically, the non-REM phase is characterized by a general slowing down of EEG activity, the appearance of specific K-complexes and carotid spindle, and in the 3rd and 4th stages by the slowest delta waves. In the 3rd and 4th stages, anabolism and synthesis of protein macromolecules occur. These last two stages are associated with the formation of a feeling of sleep satiety and subjective recovery, and they are usually observed only in the first 2-3 sleep cycles.
The REM phase is characterized by acceleration of EEG activity, rapid horizontal movements of the eyeballs, instability of the pulse and blood pressure, and paradoxical muscle hypotonia. Probably, the features of the physiological state of a person during the REM phase contribute to the processing of the cognitive and affective experience gained in wakefulness. The first REM phase appears 60-100 minutes after falling asleep. Usually, during a night’s sleep, 4-5 REM phases can be observed , the duration of which increases by the time of awakening. A person experiences 90% of dreams during the REM phase. Normally, non-REM phases account for 85% of sleep time.
How do these indicators change with sleep disturbances, which are more or less associated with depression? Sleep disturbances are observed in 95% of patients with depression. This happens:
- decreased sleep performance;
- displacement of the first REM phase in earlier hours;
- an increase in the duration of the first REM phase by reducing the 3-4 stages of the non-REM phase;
- an increase in the number and time of REM phases (over 20% of the total sleep time);
- an increase in the number of awakenings during night sleep;
- reduction in the number and total duration of the 3rd and 4th stages of the non-REM phase (up to their disappearance).
Thus, sleep becomes superficial and the person suffering from insomnia largely loses the ability to experience psychological and physical recovery and the feeling of being satiated with sleep.
Currently, benzodiazepine (BZD) hypnotics are the main means of pharmacological treatment of insomnia, regardless of its origin. However, recently an opinion has been formed about the dangers of prolonged use of these funds, moreover, many doctors speak out against their regular course taking, even for a short time.
Risk factors associated with long-term use of BZD:
- tolerance and the need to increase the dose;
- physical dependence and withdrawal symptoms;
- change in sleep formula;
- rebound insomnia (recoil syndrome);
- memory impairment, psychomotor and cognitive functioning;
- irritability and hostility.
We will not dwell on all the negative aspects associated with the intake of benzodiazepines, we will emphasize the peculiarity of their effect on the sleep formula and the mechanism of formation of rebound insomnia. BZD increase the time until the appearance of the first REM phase, reduce the number and total time of REM phases during night sleep, however, they do not significantly affect the formed ratio of different stages of the non-REM phase, moreover, it is believed that they prevent the formation of the 3rd and 4th stage of sleep. The use of BZD, while reducing the number of awakenings, may not affect the quality of recovery and saturation with sleep. When these drugs are canceled, an interesting physiological phenomenon occurs – the replenishment of the missed amount and the total time of REM phases. Consequently, a compensatory wave of increased REM phases arises, which may exceed their number in case of sleep disturbance prior to RZD appointment. This is the mechanism of rebound superficial sleep and frequent awakenings. Modern non-benzodiazepine hypnotics affect sleep architectonics in a similar way. Their preference is associated with greater safety and the absence of a direct aftereffect on the daytime functioning of the patient.
How do antidepressants work on the sleep formula for insomnia? The most common antidepressants – tricyclic (TCA) and selective serotonin reuptake inhibitors (SSRIs), similarly to benzodiazepines, inhibit the onset of the first REM phase, reduce the number and total time of REM phases, and also, probably, prevent the formation of the third and fourth stages of non- REM phase (5). The initial stage of SSRI action is associated with an increase in the number of awakenings. As a result, the effectiveness of sleep is indirectly normalized due to the relatively long-term antidepressant effect due to the general readjustment of the serotonergic system. What are the neurochemical features of the action of antidepressants associated with the effect on sleep disorders? This article will examine the features of serotonergic and antihistamine action. The above classes of antidepressants cause an increase in the activity of the entire serotonergic system due to the blockade of neurotransmitter reuptake. Antidepressants have an activating (agonistic) effect on all three subtypes of postsynaptic receptors. This action causes:
- weakening of depressive symptoms (anhedonia, circadian symptoms, vital symptoms, depressed mood);
- weakening of obsessive-phobic symptoms;
- strengthening control over impulsive actions, suppression of aggression and autoaggression (suicidality);
- weakening of drug addiction;
- easing pain;
- dyspepsia, effect on appetite.
The main antidepressant and partly anti-anxiety effects are associated with agonism to postsynaptic 5-HT 1A receptors . The increase in the activity of the other two types of postsynaptic serotonin receptors is not related to the antidepressant effect, but rather is associated with the often undesirable effects of therapy. Stimulation of 5-HT 2A receptors is associated with psychomotor activation, anxiety, insomnia, and sexual dysfunction. Stimulation of 5-HT 2 receptors increases irritability, decreases appetite, and agonism to 5-HT 3 receptors contributes to nausea and headaches. Thus, the initial effect of SSRIs can be manifested by a temporary increase in sleep disturbances and some manifestations of anxiety, which is later compensated (but not always) by a readjustment of the activity of the entire serotonergic system, which is the actual antidepressant effect. This increase in sleep and anxiety disorders can periodically exacerbate the underlying depressive symptoms.
Blockade of histamine H 1 receptors causes an increase in the effect of depressants (alcohol, barbiturates, benzodiazepines), sedation, drowsiness, weight gain, hypotension. The antihistamine effect is associated with the potentiation of falling asleep, however, it does not cause an increase in the duration of sleep and within 2-3 days this effect disappears due to the high tolerance to it.
These mechanisms have been described in connection with the emergence of new generations of antidepressants that are agonistic to 5-HT 1 receptors and block 5-HT 2 and 5-HT 3 . These drugs include trazadone, nefazadone, and mirtazapine (Remeron). The blockade of these two types of postsynaptic receptors in practice manifests itself as an independent anti-anxiety effect and rapid normalization of sleep.
The above considerations allow us to assert the uniqueness of the therapeutic action of Remeron. In addition to the well-known powerful and rapid antidepressant effect, the sleep-normalizing effect of Remeron is as follows:
- reduction in the duration and number of awakenings at night;
- restoration of the time of the onset of the first REM phase, physiological for a given patient (and not artificial inhibition), which directly therapeutically affects the circadian mechanisms in the formation and maintenance of depression;
- an increase in the total time of REM phases (in contrast to other classes of hypnotics), which prevents the appearance of rebound insomnia;
- an increase in the duration of the 3rd and 4th stages of the non-REM phase (no other drug possesses this property), which is associated with the rapid recovery of a feeling of satiety with sleep;
- an increase in the duration and effectiveness of sleep, which cannot be a manifestation of antihistamine action.
Our experience with Remeron’s therapy of sleep disorders of an affective origin confirms the theoretical foundations outlined above. Over the past year, such therapy was carried out in 26 patients suffering from insomnia, of whom only 5 had indications in the anamnesis of previous depressive conditions; 16 were between the ages of 22 and 40 and did not interrupt their work activities. None of them showed the aftereffect of the drug in the form of daytime sedation 2-3 days after the start of administration. Below we give a polysomnogram of one of the patients, recorded before and 2 weeks after taking Remeron.
The graphs show the normalization of the sequence and duration of REM phases and an increase in the 3rd and 4th stages of the non-REM phase during therapy.
In conclusion, I would like to emphasize that chronic insomnia is associated with:
- the risk of depression;
- limited contact and decreased social functioning;
- an increase in the number of visits to primary care physicians and an increase in the number of days of incapacity for work;
- the risk of accidents;
- impaired cognitive functioning;
- a decrease in the quality of life.
Different classes of antidepressants have different effects on sleep. Rapid sleep normalization contributes to adherence to therapeutic recommendations and better treatment tolerance.