Insomnia: modern approaches
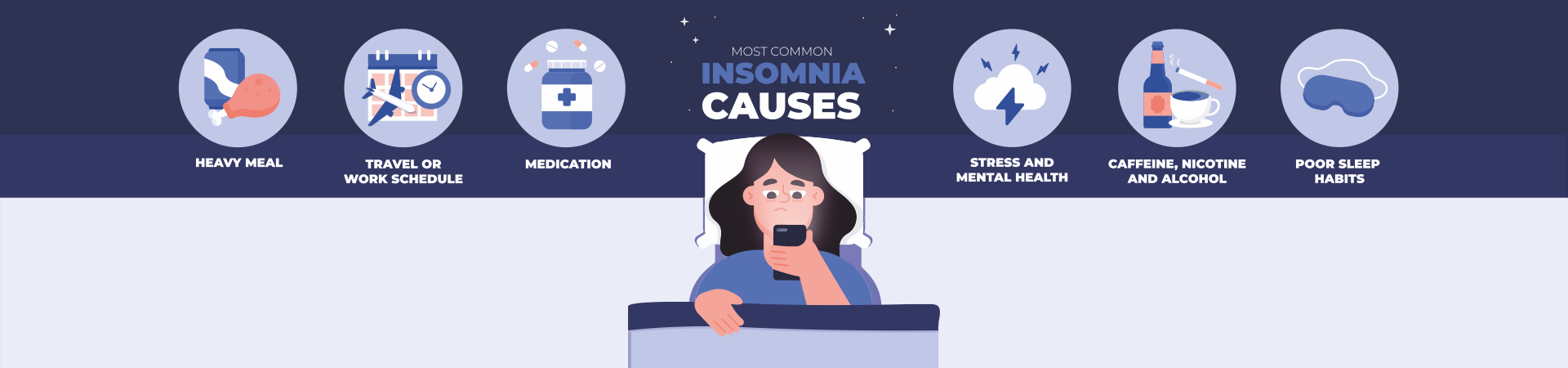
Insomnia is one of the most common sleep disorders due to difficulty falling asleep and maintaining sleep. There are three stages of insomnia: sleep disturbance (occurs most often); sleep maintenance disorder; early final awakening. There are many reasons for insomnia. The most common are psychological problems, violations of the usual regime, various diseases (of the cardiovascular system, gastrointestinal tract, etc.), as well as the use of psychotropic drugs, alcohol, coffee, overeating in the evening, especially the abuse of heavy fatty foods. Insomnia can be caused by intense mental work, noisy games, engaging reading before bed, and smoking. It should be noted that insomnia can also occur with overwork or with the constant expectation of poor sleep and related experiences, as well as with insufficient physical activity. Before proceeding to describe the clinical signs of insomnia, it is necessary to emphasize that sleep disorders can have an inorganic etiology. According to the International Classification of Diseases of the 10th revision (ICD – 10), non-organic sleep disorders mean a state of unsatisfactory duration or unsatisfactory quality of sleep, which can persist for a significant period of time, as well as difficulty falling asleep, difficulty staying asleep or early final awakening [2]. A similar approach is assumed in the ICD – 11 project [3]. The main clinical signs for making a reliable clinical diagnosis are the following: 1) a complaint about poor falling asleep and poor quality of sleep, difficulty maintaining sleep; 2) sleep disturbance occurs at least 3 times a week for at least 1 month; 3) there is a concern in connection with insomnia and its consequences, both at night and in the day; 4) unsatisfactory duration or unsatisfactory quality of sleep causes severe distress and interferes with social, professional functioning. Depending on the duration of the severity of sleep disorders, there are: • transient insomnia – duration up to 1 week. Often, this form does not require specific treatment and, as a rule, is associated with some emotion – tional experiences or changes in life; • acute insomnia – duration from 1 to 4 weeks, sleep disturbances are more pronounced. For this form of insomnia, treatment by a specialist is recommended ; • chronic insomnia – lasting more than 4 weeks. In this case, symptoms are noted 3 or more times a week. This form of the disease is characterized by a pronounced pathological change in the subjective attitude to sleep. Treatment of this form requires the mandatory intervention of specialists. According to the International Classification of Sleep Disorders (3rd Edition), the diagnosis of insomnia refers to complaints of problems starting or maintaining sleep related to daytime consequences and not related to environmental circumstances or inadequate sleep ability. With a duration of insomnia up to 3 months, this disorder is considered short-term. Insomnia is considered chronic when it persists for at least 3 months with a frequency of at least 3 times a week [4]. The European Sleep Research Society, based on the International Classification of Sleep Disorders, offers the following criteria for the diagnosis of insomnia. Criteria A-F must be met. A. The patient reports (or observes the patient’s parent or guardian) one or more of the following: 1. Difficulty starting to sleep. 2. Difficulty maintaining sleep. 3. Waking up earlier than we would like. 4. Resistance to being put to bed on an appropriate schedule. 5. Difficulty sleeping without parent or guardian intervention. B. The patient reports (or the patient’s parent or caregiver notices) that one or more of the following are associated with sleep disturbances: 1. Fatigue / malaise. 2. Impaired attention, concentration or memory. 3. Violation of social, family, professional functions or decreased academic mustache – peshnosti. 4. Violation of mood / irritability – faculty. 5. Daytime sleepiness. 6. Behavioral problems (eg, hyperactivity, impulsivity, aggression). 7. Decreased motivation / energy / initiative. 8. Predisposition to errors / accidents. 9. Anxiety or dissatisfaction with sleep. C. The reported sleep / wake complaints cannot be attributed solely to inadequate sleep capacity (ie sufficient time to sleep) or inadequate circumstances (ie the environment is safe, dark, calm and comfortable) to sleep. D. Sleep disturbance and associated daytime symptoms occur at least 3 times a week. E. Sleep disturbance and associated daytime symptoms have been present for at least 3 months. F. Difficulty sleeping / waking is not more clearly explained by another sleep disorder [5]. To objectify the diagnosis of insomnia, the Pittsburgh Sleep Quality Index (PSQI) is used – a 19-component questionnaire to assess the quality of sleep and its disorders in the range from 0 (best) to 21 (worst) points. In addition, to assess the subjective severity of insomnia, the method “insomnia severity index” is often used, which consists of 7 points, assessed on a Likert scale from 0 to 4 points. An important diagnostic tool in the examination of patients with insomnia is a sleep diary filled in by the patient within 7 days [6]. In a sleep diary, relying on subjective feelings, patients should indicate the total duration of sleep, the quality of sleep, the number of awakenings. Of the instrumental methods for diagnosing insomnia, polysomnography is used for the purpose of differential diagnosis with other forms of sleep disorders, with clinically unclear causes of sleep disorders, prolonged course and poor cure. In particular, using a sleep diary and polysomnographic examination, it is possible to identify patients with pseudoinsomnia or “sleep agnosia” (the phenomenon of distorted sleep perception) [7]. There are several effective treatments for insomnia, such as pharmacological and non-pharmacological. Non-drug treatments include stimulant therapy, sleep restriction, relaxation, sleep hygiene, and cognitive therapy. Pharmacological treatment should be in addition to non-drug therapy, most often cognitive-behavioral therapy. Despite the availability of various drugs for the treatment of insomnia, none of them can be considered ideal. Today, newer therapies are still being studied and tested in order to find a hypnotic that will have an acceptable side effect and tolerance profile , while maintaining efficacy [8]. The modern requirements for hypnotics include their high effectiveness in terms of the effect on insomnia, safety and the absence of side effects. The most common side effect of drugs with a hypnotic effect is the development of consequences when, after the normalization of night sleep, patients notice drowsiness, lethargy, and absent-mindedness during the day. In this regard, there is a constant search for optimal means that meet the specified requirements [9]. Insomnia is a direct indication for the prescription of sleeping pills. Let’s consider the main groups of drugs.
A. Z-hypnotics
These include zopiclone, zolpidem, zaleplon – non-benzodiazepine agonists of benzodiazepine receptors and GABAA receptors. Their characteristic feature is a short half-life (from 1 to 5 hours). It is believed that Z-hypnotics are less likely to cause addiction, rebound insomnia, memory and attention impairment [10].
B. Benzodiazepine drugs
These drugs act on all types of subunits of the GABA-receptor complex, causing not only hypnotic, but also other effects: anti-anxiety, anticonvulsant, sedative and muscle relaxant. In this regard, the likelihood of developing unwanted side effects when using them is higher, especially in drugs with a long half-life. In Ukraine, drugs with long half-lives (25 hours) are available, which limits their use as hypnotics.
C.
Melatonin preparations Melatonin is a hormone derived from indole and is produced primarily by the pineal gland (pineal gland) at night. It binds to specific MT 1 and MT 2 receptors, the maximum density of which is found in the suprachiasmatic nuclei of the hypothalamus (the “internal clock” of the body). The half-life of exogenous melatonin does not exceed 50 minutes. Research has shown a positive effect of melatonin supplementation on falling asleep, duration and quality of night sleep [11].
D. Blockers of histamine receptors (H 1 -blockers) Represented by diphenylhydramine and doxylamine, blocking H1-histamine receptors in the central nervous system, reducing the activity of one of the main activating systems – histaminergic. The second most pronounced effect of diphenylhydramine is anticholinergic, and therefore the possibilities of its administration are limited if glaucoma and prostate adenoma are suspected . The beneficial effects of diphenylhydramine on sleep are more about sleep maintenance than sleep initiation. Meanwhile, side effects (dizziness, impaired cognitive functions, dry mouth, blurred vision) limit the widespread use of this drug as a sleeping pill. Compared to traditional hypnotics, a feature of the action of doxylamine is the absence of a direct effect on somnogenic structures, its effect is carried out at the level of wakefulness systems by inhibiting their activity [12].
E. Antidepressants
It is believed that tricyclic antidepressants may be an effective pharmacological treatment for insomnia. They improve sleep outcome indicators, with the exception of a marked 82% increase in daytime sleepiness, which is the limiting factor in their use [13]. Trazodone is an antagonist of 5HT 2A -, 5HT 2B -, 5HT 2C -serotonin receptors and a partial agonist of 5HT 1A -receptors with serotonin reuptake inhibitor properties. The hypnotic properties of this drug are associated with the effect on H 1 -histamines, 5HT 2A -serotonin and α 1 -adrenergic receptors. Trazodone, unlike other serotonergic antidepressants, does not adversely affect sexual function and body weight. Antidepressants such as amitriptyline, mianserin, mirtazapine, agomelatine are also used to treat sleep disorders.
E. Herbal preparations
Valerian is a substance obtained from the root of Valeriana officinalis L., with an unknown main active ingredient. Valerian preparations exhibit a hypnotic effect due to partial agonism to A 1 -adenosine receptors and the GABAA-receptor complex. A clinically pronounced effect, different from the placebo effect, is achieved only with the use of the drug in high doses, while the risk of developing toxic liver damage increases [14]. No less important than the use of pharmacotherapy in the treatment of insomnia are non-drug treatments. Cognitive behavioral therapy (CBT) for insomnia is currently considered the treatment of choice and can be successfully applied regardless of causative factors. It should include psychoeducation about sleep and sleep hygiene, relaxation techniques: progressive muscle relaxation, stimulus control or sleep restriction. These methods, especially in their combined form, are evidence-based: they are as effective as pharmacological therapy in the short term [15]. However, a meta-analysis by van Straten et al. (2017) shows that the number of therapy sessions should be at least four [16]. Non-drug treatment of insomnia is considered effective if, against its background, the delay in the onset of sleep decreases or the total sleep time increases by 30 minutes. By methods corresponding to these criteria are different types of behavioral therapy, progressive muscle relaxation. Moderate regular exercise, especially in the morning, is effective enough without increasing the weakness that often bothers these patients. Also, regular water treatments can be of some benefit [17]. Compliance with sleep hygiene for mild insomnia includes the ability to relax; sleep only when tired; using the bedroom only for sleep and sexual activity; avoiding caffeine, nicotine and alcohol 4-6 hours before bedtime; reducing fluid intake before bed; avoiding heavy meals, strenuous exercise, and arousal late at night; elimination of sound sources in the bedroom, including if this source is a clock [17].
Clinical guidelines for the evaluation and management of chronic insomnia in adults recommend the following non-pharmacological therapies [18]. Stimulus control is a technique used to eliminate the negative association between bed and undesirable consequences such as wakefulness, frustration, and anxiety. These negative conditions often arise in response to attempts to sleep as a result of prolonged periods of time in bed. The goals of stimulation therapy are for the patient to form a positive and supportive relationship between bed and sleep and establish a stable sleep and wake schedule . Patients should be advised to leave bed after feeling unable to fall asleep for about 20 minutes, rather than watch for hours. Approximate instructions would be: go to bed only when you feel sleepy; stick to a regular sleep schedule; avoid naps; use the bed only for sleeping; if you are unable to fall asleep (or fall asleep again) after 20 minutes, get out of bed and relax until you become drowsy and only then return to bed. Relaxation training, such as progressive muscle relaxation or abdominal breathing, aims to reduce somatic and cognitive arousal states that interfere with sleep; can be helpful in patients with increased arousal levels and is often used in conjunction with CBT. CBT is a combination of cognitive therapy combined with behavioral treatments (eg, stimulus control, sleep restriction) with or without relaxation therapy. Cognitive therapy aims to change the patient’s inflated beliefs and unrealistic expectations about sleep. General cognitive distortions that are detected and eliminated in the course of treatment, include: “I do not I can sleep without drugs”, “Do I have a chemical imbalance,” “If I can not sleep, I have to stay – vatsya in bed and rest”, “My life will be destroyed if I cannot sleep. ” Multicomponent therapy (multimodal) uses various combinations of behavioral techniques (stimulus control, relaxation, sleep restriction) and psychoeducational measures to improve sleep hygiene. Many therapists use a multimodal approach to treat chronic insomnia. Sleep restriction initially limits the time in bed to the total sleep time that is deducted from the baseline sleep phases. This approach is designed to improve sleep continuity. As sleep time increases and the window of sleep remains limited with naps inhibited, sleep becomes more consolidated. When the continuity of sleep is significantly improved, the time in bed is gradually increased to provide sufficient sensitivity for the patient to feel rested throughout the day. In addition, this approach is consistent with cont goals – la incentives due to the fact that minimizes the amount of time spent in bed, helping to restore the link between bed and sleep. Paradoxical intention (paradoxical intention) is a specific form of cognitive therapy in which the patient is trained to confront the fear of being awake and its potential consequences. Its purpose is to eliminate the patient’s anxiety about sleep. Interaction with biofeedback teaches the patient to control certain physiological parameters through visual or auditory feedback. The goal is to reduce somatic arousal. Sleep hygiene involves educating patients about healthy lifestyle practices that improve sleep. It should be used in conjunction with stimulus control, relaxation training, sleep restraint, or cognitive therapy. It is also important to stick to a regular schedule, have a healthy diet and exercise during the day, avoid sleep, caffeine, other stimulants, nicotine, alcohol, excess fluids, or stimulation of activity before bed.