What is insomnia in plain language
Insomnia (I) is a disorder associated with difficulty initiating (starting) and / or maintaining sleep. The term “insomnia”, often used even by doctors, is inadequate, since objective studies do not reveal a complete lack of sleep in patients who have presented such complaints. Acute, subacute and chronic I. According to the severity – mild, moderate and pronounced. Clinical phenomenology of I includes presomnic , intrasomnic, and post-somnic disorders. Presomnic disturbances are difficulties in starting to sleep, with the most common complaint being difficulty falling asleep; with a prolonged course, pathological “rituals of going to bed”, as well as “fear of bed” and fear of ” sleep failure ” can form . The arising desire to sleep disappears as soon as the patients are in bed, painful thoughts and memories arise, motor activity increases in an effort to find a comfortable position. The onset of drowsiness is interrupted by the slightest sound, physiological myoclonus . If falling asleep in a healthy person occurs within a few minutes (3-10 minutes), then in patients it sometimes takes up to 120 minutes or more. A polysomnographic study (Fig. 1) of these patients showed a significant increase in the time to fall asleep, frequent transitions from stages 1 and 2 of the first sleep cycle to wakefulness. Often, falling asleep by patients is ignored and all this time is presented to them as continuous wakefulness. Intrasomnic disorders include frequent nocturnal awakenings, after which the patient cannot fall asleep for a long time, and sensations of “shallow”, “shallow” sleep. Awakenings are caused by both external (primarily noise) and internal factors (frightening dreams, fears and nightmares, pain and autonomic shifts in the form of breathing disorders, heart palpitations, urge to urinate). All of these factors can awaken healthy people who have good sleep. But in patients, the threshold of awakening is sharply reduced and the process of falling asleep after an episode of awakening is difficult. The decrease in the threshold for awakening is largely due to insufficient depth of sleep. Polysomnographic correlates of these sensations are the increased representation of the surface stages (1 and 2 FMS), frequent awakenings, prolonged periods of wakefulness within sleep, reduction of delta sleep, and increased motor activity (Fig. 1).
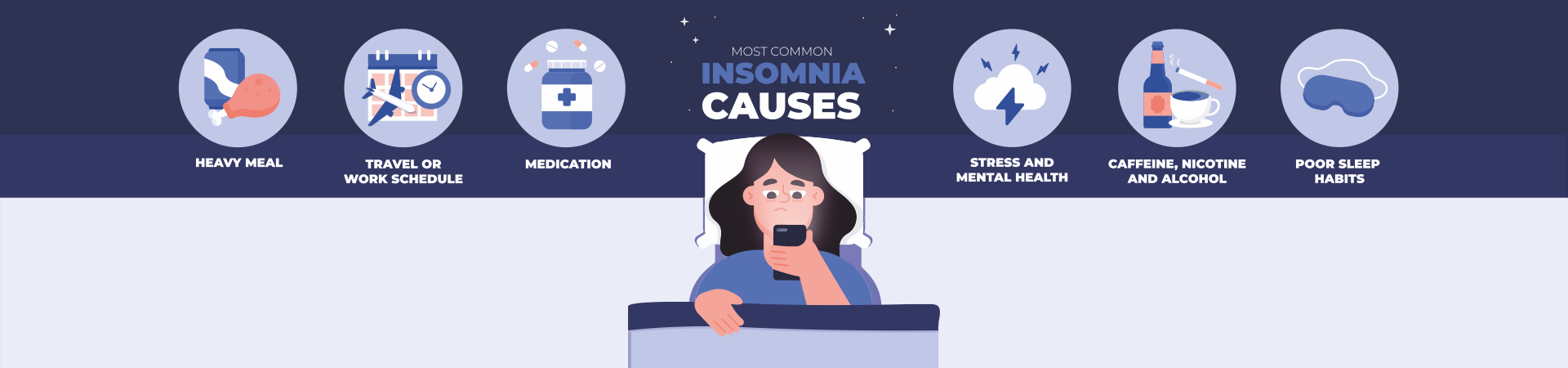
Post-somnolent disorders (disorders that occur in the immediate period after awakening) are a problem of early morning awakening, reduced performance, “weakness”. Patients are not satisfied with sleep. Non- urgent daytime sleepiness can also be attributed to post-somnolent disorders. Its peculiarity is the difficulty of falling asleep even in the presence of favorable conditions for sleep. Often, patients complain of too short sleep, without specifying the problems of starting or maintaining sleep, and at least 20% of those suffering from insomnia indicate a subjective sleep duration of less than 5 hours. This figure is important for both patients and doctors, as it seems to reflect a kind of physiological minimum sleep during the night. The relationship between subjective sleep assessments and its objective characteristics is ambiguous, although more often they coincide. Meanwhile, sometimes patients complain of a complete lack of sleep for many nights, however, with an objective polysomnographic study, sleep is not only present, but its duration exceeds 5 hours (sometimes reaching 8 hours), and the structure of sleep is not too deformed. This situation is defined as distorted sleep perception (or “sleep agnosia”). More often, a similar phenomenon is observed in patients with mental illness. It should be emphasized that in such cases, the appointment of sleeping pills (especially with a sleep duration of 6 hours or more) is not rational. The reasons are diverse: 1) stress (psychophysiological insomnia ), 2) neuroses, 3) mental illness; 4) somatic diseases; 5) psychotropic drugs, 6) alcohol, 7) toxic factors, 8) endocrine-metabolic diseases, 9) organic brain diseases, 10) syndromes that occur during sleep (sleep apnea syndrome; movement disorders during sleep), 11) pain phenomena , 12) unfavorable external conditions (noise, humidity, etc.), 13) shift work, 14) change of time zones, 15) impaired sleep hygiene.
Insomnia treatment involves two approaches. The first, the most appropriate, is to eliminate the factors that cause insomnia . The second one includes measures to normalize sleep itself. The general tactics are as follows: 1) in the early manifestations of sleep disorders, the first approach dominates; 2) with extensive and long enough insomnias – a combination of both approaches; 3) in chronic insomnias , when the factor that caused them has become less relevant, the second approach dominates. Pharmacotherapy And includes drugs of different chemical groups. The most effective and safe drugs are currently considered to be those with a short (less than 5 hours) and medium duration (from 5 to 15 hours) half -life . These include, first of all, imidazopyridines (international name zolpidem , commercial name Ivadal), cyclopirrolones (international name zopiclone , commercial names Imovan, Somnol , Piclodorm ) and, secondly , benzodiazepines (international names midazolam , triazolam ). Ethanolamines (international name doxylamine , commercial name Donormil ) and melatonin are also used .
In addition to pharmacological methods, psychotherapy, acupuncture, encephalophony ® (“Music of the Brain” ® is a method based on obtaining individual music of a person from his electroencephalogram), phototherapy (treatment with bright white light), herbal medicine are used in the treatment of I. When sleep apnea syndrome is identified as the cause of I, the most effective treatment of breathing disorders during sleep with the help of devices that create a constant air flow ( CPAP or BayPAP ).